The Koller Working Group
The research work of this group focuses on gene and cell therapy. In gene therapy, functioning genes are either introduced into human cells, or defective genes are repaired.
Gene therapy is the only way to combat the root cause of Epidermolysis Bullosa. If we look at the path from the affected gene to the resulting defective protein (e.g. type VII collagen), we can see that an improvement of the disease characteristics can be achieved by gene correction at the DNA or RNA levels. A one-time application with a long-term effect is achieved if the gene is corrected on the DNA level.
In the classic ex vivo* gene replacement therapy, the mutated gene is supplemented by a healthy gene copy introduced into the cell. Using this method, the EB House has also helped with the successful treatment of patients who have junctional EB. The healing of the transplanted skin areas was achieved by transplanting corrected, stable skin into these areas.
Nowadays, we can also repair gene mutations with pinpoint precision in the genome, thanks to the development of “designer nucleases”. Pinpoint precision here means without introducing an additional gene copy, but repairing directly in the existing genome of the cell.
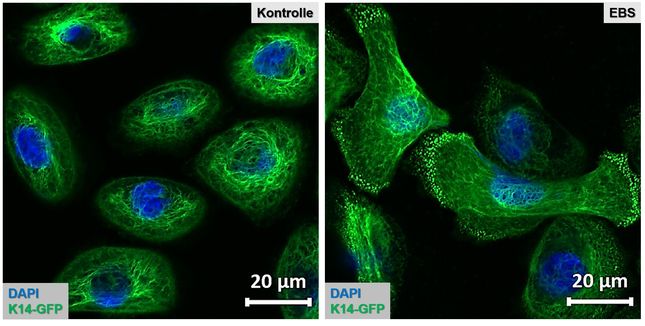
In our WG, we use the designer nucleases CRISPR/Cas9 and TALEN to deactivate or correct mutated genes in targeted manner, thus developing an alternative and very safe approach to gene therapy. We are currently creating specific nucleases for the EB-associated genes COL7A1 (collagen 7), COL17A1 (collagen 17) and KRT14 (keratin 14) – and we have already successfully tested these in patient cells.
In addition to the efficiency of this method, safety is also an essential aspect in terms of clinical use. We are using the safest ‘gene editing’ tools available today to take another step towards our goal – the broad-based use of gene therapies for EB.
A second therapy approach for EB established in the laboratory could possibly be used in vivo** as well. It is based on the elimination of mutations at the RNA level. In recent years, this method, called “SMaRT” for short, has already been successfully used in the laboratory to correct EB-associated genes. We are currently working intensively on the question of how and in which form we can introduce the repair molecules (RTMs) directly into the skin.
The choice of the above gene therapy methods depends on the particular EB form and the type of mutation. However, the chosen therapy method must ultimately be able to unite two essential aspects – efficiency and safety!

„Our vision is the development of an efficient and safe therapy option using nucleases. We want to create a simple therapy that can be adapted to any genetic modification in order to treat as many patients as possible.”
Ulrich Koller, PhD, Head of the Koller Working Group
Team: Ulrich Koller, PhD (Team Leader); Thomas Kocher, PhD; Stefan Hainzl, PhD; Johannes Bischof, PhD; Bernadette Liemberger, MSc; Janine Zwicklhuber, BSc
GOOD TO KNOW:
*Ex vivo gene therapy: The laboratory introduction into or correction of genes in cells that have previously been removed from a human being and are consequently returned to the human being for the treatment of a genetic disease, either through transplantation, infusion or injection.
**In vivo gene therapy: The correction of genes directly in the tissue or in an organ of a human being in order to treat a genetic disease.